Learn about good design
Educational Updates
We update the articles daily - stay tuned!
check out our Articles

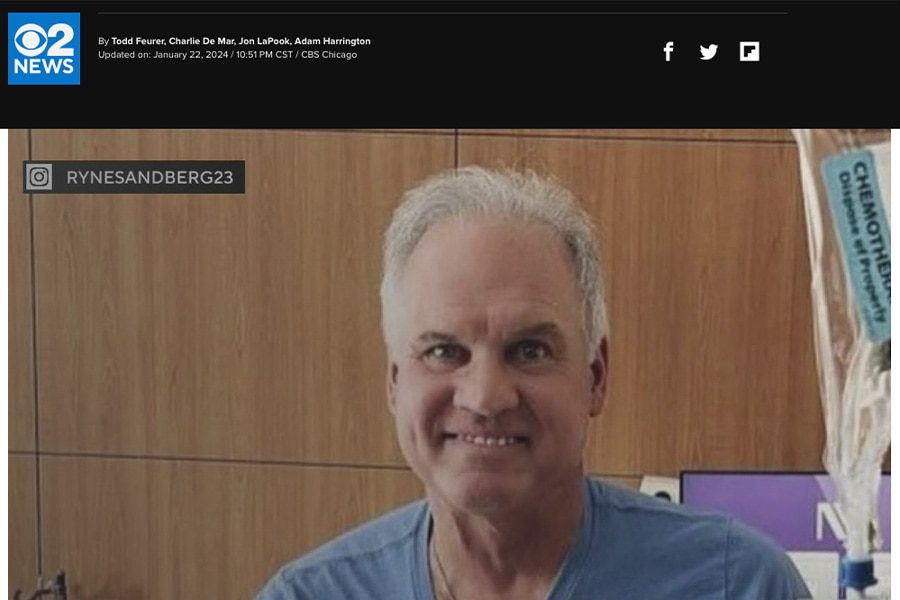
Dr. Moran Comments on Ryne Sandberg’s Cancer Announcement
January 23, 2024
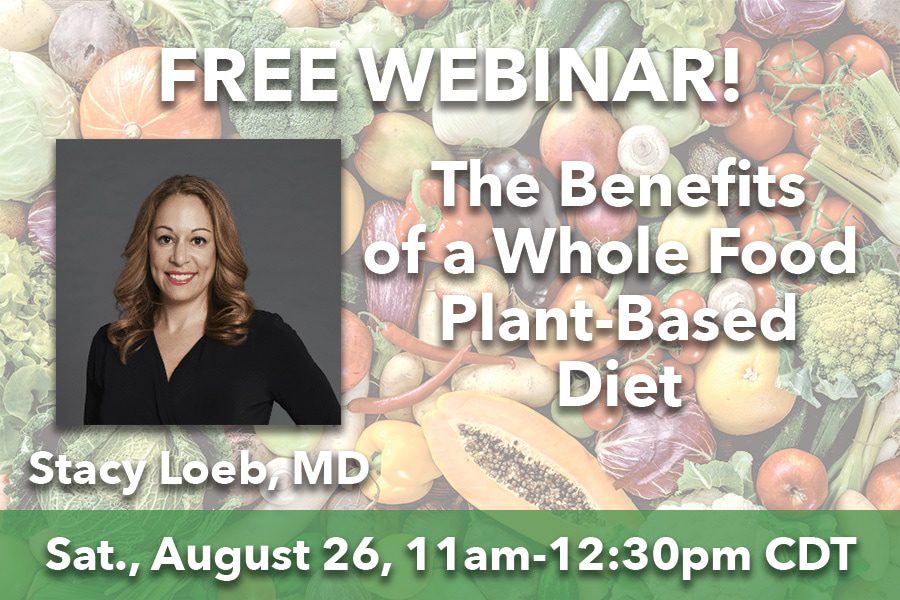
Free Webinar – the Benefits of a Whole Food Plant-Based DIet
August 23, 2023


Female Friday Funday Float 2023
July 18, 2023